A probe-based, minimally invasive surgery using a laser system may change how neurosurgery will be performed in the future. The technique is having immediate impact on some patients with deep-seated or inoperable brain tumors. According to Eric Leuthardt, MD, a Washington University neurosurgeon at Barnes-Jewish Hospital and the Siteman Cancer Center, early results suggest the surgery has the ability to extend lives.
“We are giving people with glioblastomas and high-grade tumors better outcomes with less morbidity” says Leuthardt of the ablation surgeries he performs with a system known as NeuroBlate, which is FDA-approved for neurosurgery. According to Leuthardt, Barnes-Jewish is the third hospital in the nation to have the laser system.
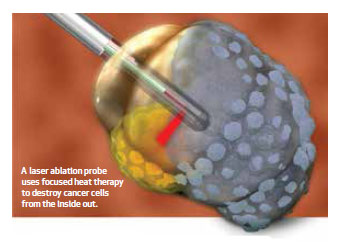 The system delivers focused heat therapy to tumors while sparing surrounding healthy tissue. Surgeons achieve these results by using the system in coordination with intraoperative MRI scanning, real-time imaging and a fiber-optic probe with a unidirectional laser. Specifically, it delivers laser interstitial thermal therapy. As the laser reaches a temperature between 48 and 52 degrees Celsius, it heats and destroys the cancer cells from the inside out.
The system delivers focused heat therapy to tumors while sparing surrounding healthy tissue. Surgeons achieve these results by using the system in coordination with intraoperative MRI scanning, real-time imaging and a fiber-optic probe with a unidirectional laser. Specifically, it delivers laser interstitial thermal therapy. As the laser reaches a temperature between 48 and 52 degrees Celsius, it heats and destroys the cancer cells from the inside out.
“The procedure is relatively well-tolerated, and our patients go home quickly,” says Leuthardt, who also is director of Washington University’s Center for Innovation in Neuroscience and Technology.
Key indications for the procedure include inoperable brain tumors in the thalamus or insula, recurrent metastases after stereotactic radiation, recurrent glioblastomas and radiation necrosis that has led to swelling. But patients whose only other surgical option is biopsy may also be candidates for the procedure, Leuthardt says.
While treatment is rendered in bursts lasting seconds to minutes, the full procedure takes five to six hours to complete due to the precise brain mapping needed to plot the path of the probe. Treatment is accomplished with the patient situated in an intraoperative MRI device. A single-use miniframe that is MRI-compatible is mounted to the patient’s head to help determine probe placement.
The procedure requires a 2- to 3-millimeter incision and a burr hole about the size of a pencil’s diameter. A narrow probe with a fiber-optic laser is inserted through the burr hole into the center of the tumor. The unidirectional ability of the probe, coupled with real-time imaging, allows the surgeon to create heat fields that conform to the shape of the tumor and destroy it. “You can actually watch the heating and laser shots as they occur,” Leuthardt says.
“Patients tend to go home a couple of days after surgery compared to being in the hospital for a week with the standard surgical approach. And the outcomes that we are seeing, at least very early on, are encouraging for aggressive tumors like glioblastomas,” Leuthardt says. “Without question we can provide a surgical option for people who may not otherwise have one.”
Leuthardt is one of eight neurosurgeons in the nation using the laser ablation system.