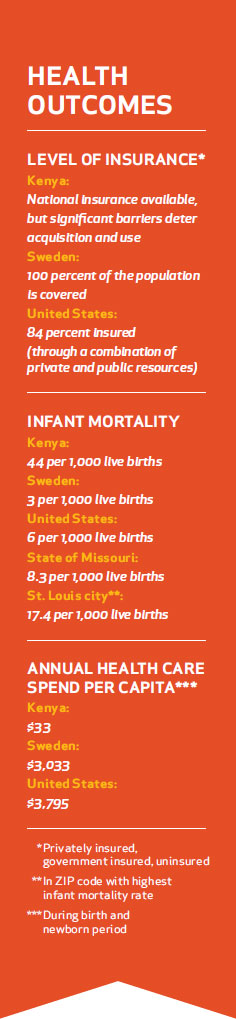
Maternal and infant health care outcomes in St. Louis city and county illustrate this disparity. If a person standing in the urban setting surrounding Barnes-Jewish Hospital and St. Louis Children’s Hospital throws a baseball one ZIP code to the north, it will hit health care outcomes not altogether different from those in sub-Saharan Africa. If the ball is thrown to the west, it will hit outcome rates more like those in Scandinavia. (See the Health Outcomes table on page 6.) Only a few of the reasons for these drastic differences in maternal and infant health outcomes have medical causes; most are driven by a complex combination of social and economic issues. Among the major barriers to healthy outcomes are poverty, health literacy, malnutrition, access to health care and the transportation needed to receive it.
Health Outcomes in Sweden and Kenya
Swedes consider health care a basic civil right, regardless of an individual’s socioeconomic status. In Sweden, the infant mortality rate is three per 1,000 infants, and the country is ranked fifth in the world for best infant mortality outcomes, according to the Factbook.
In Kenya, where infant mortality is very high—44 per 1,000 live births— the challenges to maternal-newborn wellness are great. Due to the scarcity of health care facilities and a lack of transportation to those facilities that do exist, more than 50 percent of Kenyan women deliver at home, with or without a trained birth attendant.
While Kenya does offer national health care to all children younger than age 5, transportation to that care is costprohibitive, even for those living in cities. Given the significant challenges faced in Kenya, nearly 13 percent of all children die before the age of 5.
Improving Outcomes
According to Sweden's Ministry of Public Health, health care is available to all of that country’s citizens from cradle to grave. UNICEF data pertaining to Sweden reveal that:
- All Swedish women have access to preconception health care. A total of 98.5 percent of women in the country attend the recommended course of prenatal visits.
- Advanced-practice nurses help reduce the cost of health care while improving the continuity of care for newborns. At birth, every child is assigned to a nurse managed medical home. An assigned nurse serves as a third parent, ensuring the child receives excellent preventive care.
- Each health care provider is measured using a scorecard that shows his or her performance compared with other providers in the same city, the county and the country. All nurses and physicians are facile with local and national rankings.
In Kenya, local groups, some supported by international aid, are organizing to improve maternal-newborn health care. For example, the “Umama Salama,” or Safe Motherhood, program is a partnership between Lwala Community Hospital, in Lwala, Kenya, and the area's traditional birth attendants. The primary intent is to encourage women to travel to the hospital to deliver. Since the program began, infant mortality has improved by an estimated 50 percent.
In the United States, the Affordable Care Act (ACA), upheld in June by the Supreme Court, is intended to increase the total number of insured individuals from the current 84 percent of Americans to 94 percent within 10 years. While all pregnant women are already entitled to Medicaid coverage from the time pregnancy is confirmed through six weeks postpartum, the ACA will ensure that more women have the option to obtain care from preconception to beyond the postpartum period.
The Local Perspective
In St. Louis, community health organizations and providers, convened locally by the Maternal, Child and Family Health Coalition and the Integrated Health Network (IHN), are partnering in a regional initiative to seek funding through the Strong Start for Mothers and Newborns grant from the Center for Medicare and Medicaid Innovation (CMMI). The grant itself stands as an example of the national movement toward an emphasis on public health and prevention. CMMI offers more than $40 million in grant funding for initiatives aimed at reducing preterm birth, and the regional initiative seeking funding is composed of representatives from multiple organizations, including several that are business competitors.
A regional group, led by the IHN, will work to increase the number of providers that offer group prenatal care in St. Louis and enhance the care offered. The Women's Health Clinic, with 11 years of experience offering group prenatal services, will receive funding to improve the existing program and will act as a resource site for new providers.
On the campus shared by Barnes-Jewish Hospital, St. Louis Children’s Hospital and Washington University School of Medicine, efforts are increasing to reduce poor perinatal outcomes. This work includes improved communication between providers and patients, ongoing research and implementation of change using evidence-based education, and development of partnerships with community-based organizations and initiatives that share the goal of improving maternal-newborn health.
Outpatient Care
The Ob/Gyn Clinic at Barnes-Jewish Hospital, working in close coordination with community agencies and schools, provides women with the preconception, prenatal and postnatal care that too often can be insufficient for vulnerable populations. Ongoing and new programs are aimed at improving care continuity and health literacy, as well as perinatal outcomes for mothers and babies.
Centering Care
The Centering Pregnancy initiative runs on a model of group-centered health care, whereby pregnant women receive prenatal care, education and support in a group setting. The Teen Pregnancy Center Ob-Gyn Clinic at Barnes-Jewish Hospital is one venue for Centering Pregnancy. The center implemented this care model in 2001 and expanded to serve low-risk adult women in 2009.
The program annually serves 150 low-risk pregnant teens and adult women. The center has seen a significant decrease in rates of preterm birth and low birth weight among participants. By using Centering Pregnancy, the center has increased patient satisfaction scores as compared to those from women who are treated using the traditional prenatal-care model.
Health Literacy Initiative
The Health Literacy Initiative, begun in the spring of 2011, is a five-year strategic plan to improve clear communication between patients and health care staff within the Barnes-Jewish Ob-Gyn Clinic.
Outpatient and Inpatient Care
The Fetal Care Center at Washington University Medical Center is designed to serve pregnant women and their families whose fetus is diagnosed with any kind of anomaly. It provides evidence-based, patient- and family-centered, coordinated, multidisciplinary maternal, fetal and pediatric care for all who need it.
Barnes-Jewish Hospital, St. Louis Children’s Hospital and Washington University School of Medicine provide and are continuously working to improve world-class health care for both low- and high-risk births and newborn inpatient care. These entities participate in ongoing training to implement the patient- and family-centered care model, improve cultural competency and participate in training that emphasizes the use of best evidence to inform practice. Women and Infants Services at Barnes- Jewish Hospital supports communityoutreach programs, including health fairs and educational events for both health professionals and the broader community. Additionally, health care professionals at St. Louis Children’s Hospital continuously work to improve existing programs and implement new community-outreach initiatives, including the successful asthma and dental mobile outreach initiatives, as well as a variety of safety-related programs.
Improving Care Through Research
The Women and Infants Health Specimen Consortium (WIHSC) collects specimens and patient medical data longitudinally throughout gestation from the mother and, after delivery, from the infant. These mother-infant sets of data are recorded, stored and made available to investigators. The consortium has formed the central infrastructure critical for the Washington University academic community to actively engage in research focused on many of the clinically important issues in women's health. Those issues include: pregnancy-specific reference intervals, pre-eclampsia, recurrent pregnancy loss, preterm delivery and other adverse pregnancy outcomes, many of which are more common in and lead to worse outcomes among the underinsured and uninsured.
Resources
CIA Factbook: https://www.cia.gov/library/publications/ the-world-factbook/index.html
Center for Medicare and Medicaid Innovation: http://bjhne.ws/cw
Fetal Care Center: fetalcare.org
St. Louis Maternal, Child and Family Health Coalition: http://bjhne.ws/cx
Umama Salama: http://bjhne.ws/cv
Women and Infants Health Specimen Consortium: research.wustl.edu/core-facilities/wihsc/