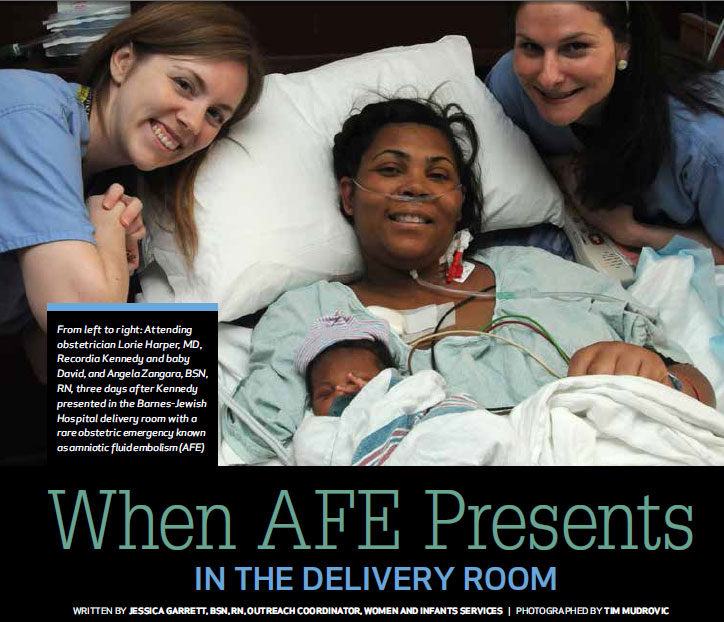
Recordia Kennedy’s first three deliveries in 1991, 1994 and 1996 were as uneventful as birth can be in terms of her own health. “And I have always been a healthy person,” says Kennedy, age 41, just five days after she nearly died during her fourth delivery, due to the rare obstetric emergency known as amniotic fluid embolism (AFE), or anaphylactoid syndrome of pregnancy.
“A combination of maternal fetal medicine (MFM), great obstetrical nursing and phenomenal medical care saved her life,” says Washington University physician and Barnes-Jewish Hospital Women and Infants Medical Director George Macones, MD. Macones points to excellent teamwork, a timely forceps delivery and the use of an unusual combination of resuscitative medications as some of the causes of the unexpected recovery for mother and baby.
While Kennedy has asthma and had a placenta previa with this pregnancy that resolved in early January 2012, she seemed healthy on Feb. 26, according to Angela Zangara, BSN, RN, her bedside nurse that day. Kennedy was progressing in labor, with an epidural infusing. The fetal heart tracing was NICHD Category II, and she was approaching the second stage of labor quietly, without pain. Then, “She called out, thinking the baby was ready to deliver,” says Zangara, who, along with Barnes-Jewish Hospital resident physician Julianna Verticchio, MD, checked Kennedy’s cervix. “She was eight [cm],” Zangara says, “so we sat her back up.”
That’s when things started to deteriorate for Kennedy, Zangara says. “She said, ‘I feel like I can’t breathe.’ She coughed for about 10 seconds, like she couldn’t get air in.” Zangara checked the pulse oximeter reading. “It went from 98 to 81, and then she went unresponsive.” Zangara called out Kennedy’s name multiple times with no response, then performed a sternal rub while Verticchio pushed the emergency code button.
Carolyn Mank, BSN, RN, responded to the call and, after finding no carotid pulse, started chest compressions within one minute. “There was no chaos,” Mank says. “We can respond with urgency and instinct in OB because we are so used to working stat.”
Barnes-Jewish Hospital attending obstetrician and Washington University maternal fetal medicine fellow Lorie Harper, MD, was leaving the operating room following a cesarean section when she received the obstetric emergency page.
“The patient was pulseless, and there were no fetal heart tones when I walked in,” Harper says.
Within two minutes of being at the bedside, Harper had climbed onto the lower half of the bed into a kneeling position and delivered Kennedy’s baby boy using Simpson-Luikart forceps from a +2 station, while Zangara applied suprapubic pressure. “Luckily she was complete by that time,” Harper says. If she had not been complete, Harper says, an emergent, bedside cesarean section would have been indicated.
Mank and others continued chest compressions. The obstetric anesthesia team had arrived with Harper and had successfully intubated Kennedy concurrent with delivery. “I heard the baby crying in the room, and our working differential was already AFE versus pulmonary embolism” Harper says.
The acute care team arrived immediately after delivery, and the full code continued, with the maternal fetal medicine, obstetric nursing and anesthesia teams working together, each maintaining a vital role in Kennedy’s medical management and resuscitation. “Everyone knew what their responsibility was and not only performed well, but also kept the rest of the team up to date,” says Tim Nienhaus, RN, the responding nurse from the acute care team.
Excellent teamwork was integral to Kennedy’s successful resuscitation.
“The patient would have died if there had been three separate tornadoes going on in that room,” Macones says.
Approximately 30 minutes into the ACLS-compliant code, when hope for Kennedy’s successful resuscitation was dwindling, the anesthesiology team gave four embolus-specific medicines, concurrently maintaining the ACLS algorithm, according to Maryann Otto, MD, Washington University anesthesiologist at Barnes-Jewish Hospital. “Within minutes of receiving those meds she got a pulse back,” says Otto, who led the team that managed Kennedy's airway during the code.
According to Otto, AFE occurs when amniotic debris enters maternal circulation and causes the release of endogenous serotonin mediators. Because AFE does not naturally occur in animals, and scientists cannot recreate the entire picture of AFE in laboratory animals, consideration of treatment for AFE comes from research done on the chemical mediators of serotonin involved in pulmonary embolism [PE]. “With PE, there is the additional component of mechanical obstruction to consider. With AFE, there is no mechanical obstruction. Therefore, the focus of treatment is on the chemical mediators of serotonin. A sudden imbalance in these mediators causes a cascade that leads to extreme pulmonary vaso- and broncho-constriction,” Otto says. “This extreme pulmonary hypertension leads to right-sided heart failure and, quickly, to cardiac arrest.”
The estimated incidence for AFE is two per 100,000 deliveries, according to a population-based cohort study performed by Knight, et. al., published in 2010 in Obstetrics and Gynecology. However, the incidence reported in recent medical literature ranges from two to 7.7 cases per 100,000 deliveries. While it is very rare, it is estimated that AFE caused between 5 and 15 percent of all pregnancy-related deaths in developed countries between 1999 and 2009, according to an evidence-based review by Conde-Audelo and Romero, published in the American Journal of Obstetrics and Gynecology in 2009.
AFE presents suddenly, with 56 percent of cases occurring before or during labor and the remaining 44 percent occurring within four hours after delivery.
The reported mortality rate associated with AFE varies widely. In addition to finding a 20 percent fatality rate, the Knight study showed that a greater percentage of the women who died were from ethnic-minority groups.
Kennedy was at increased risk for antenatal AFE related to multiple factors. There is no documented evidence that she experienced any of the premonitory symptoms until just before her cardiac arrest. Kennedy does not remember the day of her delivery, and family members present at the time of her respiratory depression and cardiac arrest state she had not mentioned any symptoms until just prior to losing consciousness.
Clinically, there are two major components to look for with AFE, says Harper. They are cardiopulmonary depression or arrest and disseminated intravascular coagulation (DIC). There is no diagnostic blood test; in the moment, the team must use clinical presentation to diagnose AFE, then treat accordingly while resuscitating. If the baby is still in the uterus when AFE occurs, the obstetric team has less than five minutes from the moment of cardiac arrest to maximize the chance for the baby to be born neurologically intact, says Harper.
Newborn David has done well. He earned a five-minute Apgar of 9, had an umbilical arterial blood pH of 7.22 and went home on day of life 5 instead of 3 or 4, due only to the need to remain in-hospital with his mother.
Kennedy went on to exhibit all of the entry criteria for AFE. “Basically, as soon as she had a pulse again, she was bleeding from every possible site,” says Mank of the ensuing DIC. Kennedy was moved to the medical intensive care unit (MICU). The obstetric team placed a Bakri balloon in Kennedy's uterus to help with her DICrelated bleeding from that site, and her coagulopathy was managed in cooperation with the MFM and MICU medical teams. During her hospital stay, Kennedy received a total of 23 units of blood products for acute DIC with, at one point, an undetectable fibrinogen. Her recovery has been slow but steady, with a few complications, including the development of a deep venous thrombosis (DVT) during her inpatient hospital stay.
Just 17 days after she nearly died giving birth, Kennedy returned home to care for her newborn and three older children.
She has some physical limitations that are believed by her physicians to be temporary, but she is still struggling to speak and walk as well as she used to. “I’m going to have to try hard just to keep up,” she says, then looks away.
“She is doing well,” says Margaret Baum, MD, the obstetrician who cared for Kennedy prenatally and has treated her since discharge from the hospital. “I’ve seen her two or three times; she sees us for routine medical care. Her gait and memory are improving,” Baum says, noting that Kennedy has been walking independently, though at times unsteadily, all along. “She’s not on dialysis, her last creatinine was normal, and her liver function tests are almost normal.” According to Baum, Kennedy also regularly sees an internal medicine physician for continuing anticoagulation and monitoring of her renal dysfunction and the neurological sequelae of extended resuscitation.
Kennedy says that although she has strong and steady family support, the recovery has been emotionally and physically difficult.
But this is not the first challenge that Kennedy, who spent some of her formative years without a guardian, has faced. And she is inspired and determined to recover. “I have a new baby,” she says. “I will never take life for granted.”